Gamma Knife radiosurgery is a highly precise, noninvasive form of stereotactic radiosurgery used primarily to treat disorders of the brain. Despite its name, Gamma Knife does not involve an incision or a blade. Instead, it delivers focused beams of gamma radiation to a specific target within the brain, allowing physicians to treat complex neurological conditions with remarkable accuracy while minimizing damage to surrounding healthy tissue.
Overview and Historical Development
Gamma Knife radiosurgery was developed in the mid-20th century by Swedish neurosurgeon Lars Leksell, who sought an alternative to open brain surgery for deep or high-risk lesions. The technique combines principles of neurosurgery, radiation oncology, and advanced imaging. Over decades of refinement, Gamma Knife has become a cornerstone in the management of many intracranial conditions, particularly those that are small, well-defined, or surgically inaccessible.
How Gamma Knife Radiosurgery Works
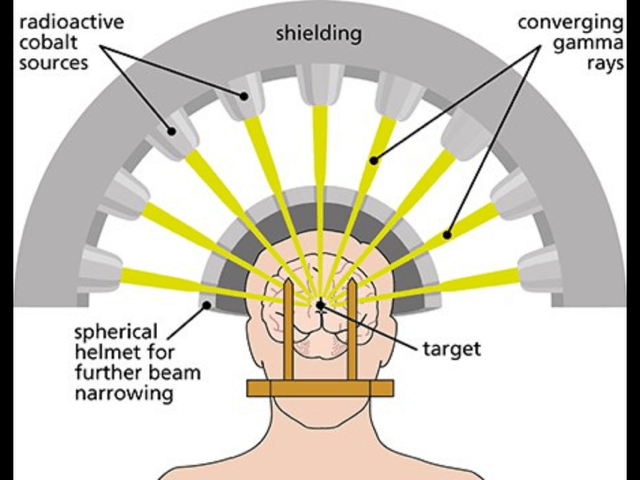
Gamma Knife uses about 200 small, individually weak beams of gamma radiation—typically from cobalt-60 sources—that converge precisely at a single focal point. Each beam alone is harmless to the tissue it passes through, but where the beams intersect, a high dose of radiation is delivered to the target. Thus, a ‘lethal’ dose of radiation is delivered to the target tissue, killing it; but the surrounding tissues are spared excessive radiation. Obviously, in the brain, sparing the surrounding normal brain from trauma is a great idea.

The procedure begins with stereotactic localization. Traditionally, a rigid head frame is secured to the patient’s skull to ensure sub-millimeter accuracy, though newer systems may use frameless mask-based immobilization for select cases. High-resolution imaging, such as MRI or CT scans, is then used to identify the lesion. Specialized planning software allows clinicians to shape and tailor the radiation dose to the exact size and geometry of the target. Accuracy of delivery with the frame is measured at about .25 millimeters.
Treatment is usually completed in a single session and can last from minutes to a few hours, depending on the complexity of the case. There are select cases that are treated in several installments over a few days. They generally use the frameless mask based system.
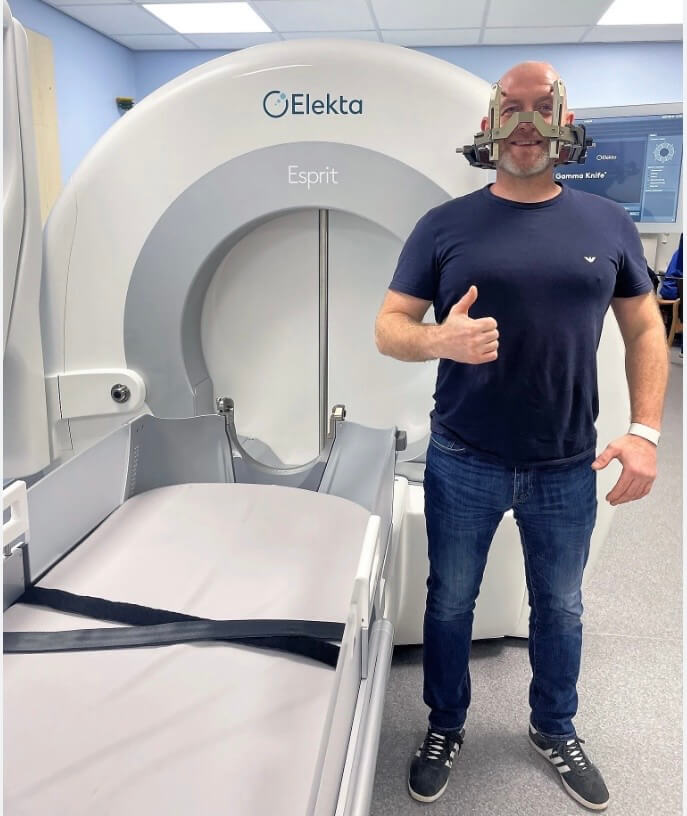
Gamma Knife is a multidisciplinary treatment involving Neurosurgeons, Radiation Oncology and Physicists. It is highly technical and precise. While there may be some brief, minor pain as the frame is applied (we numb the skin) the treatment itself is painless and does not require general anesthesia. Some patients will have a minor sedative administered just to help them be calm and sleep. You leave the center the same day and recovery is 1-2 days.
Clinical Indications
Gamma Knife radiosurgery is used to treat a wide range of neurological conditions, including:
- Benign and malignant brain tumors, such as meningiomas, acoustic neuromas, and brain metastases that have spread from cancer that started elsewhere in the body.
- Vascular disorders, including arteriovenous malformations (AVMs) and cavernomas.
- Functional disorders, such as trigeminal neuralgia and selected movement disorders
- Residual or recurrent disease after conventional surgery or radiation therapy
Its precision makes it particularly valuable for lesions located near critical brain structures where open surgery would carry significant risk.
Advantages of Gamma Knife Radiosurgery
One of the greatest advantages of Gamma Knife is its noninvasive nature. Because no incision is required, patients avoid many of the risks associated with open surgery, such as infection, bleeding, and prolonged hospitalization. Most patients are treated on an outpatient basis and return to normal activities within one or two days.
The accuracy of Gamma Knife also allows for high radiation doses to the target while sparing surrounding brain tissue, reducing the likelihood of cognitive or neurological side effects. For many conditions, local control rates are comparable to—or better than—those achieved with traditional surgery or fractionated radiation therapy.
Risks and Limitations
Although Gamma Knife is generally safe, it is not without risks. Potential side effects include headache, fatigue, nausea, or transient neurological symptoms. In some cases, delayed radiation effects such as swelling or radiation necrosis can occur, requiring medical management.
Gamma Knife is also limited to intracranial targets and is most effective for relatively small lesions. (Less than 3 cm is optimal). Large tumors or conditions requiring immediate decompression may still require open surgery.

The ability for Gamma Knife to work is based on the imaging accuracy of the lesion and targeting that lesion. If the lesion has vague edges or targets poorly, success is reduced.
Finally, because Gamma Knife does not cut out the target, it is possible for it to regrow and come back. We will try and quote you fairly specific rates for this. Some are very, very low; some are higher.
Conclusion
Gamma Knife radiosurgery represents a major advancement in modern neurosurgical and oncologic care. By combining precise imaging, advanced computer planning, and focused radiation delivery, it provides an effective and minimally invasive treatment option for a wide range of brain disorders. As technology continues to evolve, Gamma Knife remains a powerful example of how innovation can improve outcomes while reducing risk and recovery time for patients with complex neurological conditions.