Radiofrequency ablation (RFA) is a minimally invasive medical procedure used to reduce pain or destroy abnormal tissue by applying controlled heat generated from radiofrequency energy. It is most commonly used in pain management, cardiology, oncology, and vascular medicine. By selectively targeting specific nerves or tissues, RFA can provide long-lasting symptom relief while avoiding the need for major surgery. It is commonly performed in an ASC and takes about 30-60 minutes. Recovery is 1-2 days only as the procedure is done thru needles and probes inserted thru those needles only (no incisions).
Principles & Mechanism
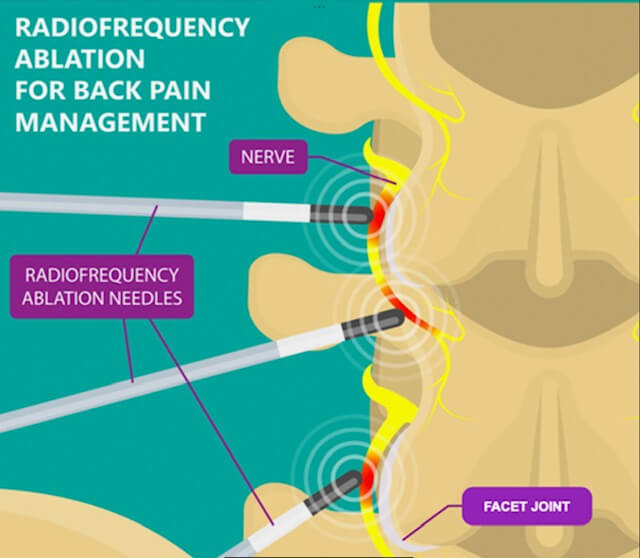
Radiofrequency ablation works by delivering high-frequency alternating electrical current through a specialized needle or catheter. This current generates heat at the tip of the device, typically reaching temperatures between 60°C and 90°C. The heat causes thermal coagulation, which disrupts nerve conduction or destroys targeted tissue while sparing surrounding structures. When used for pain control, RFA interrupts pain signals by disabling small sensory nerve fibers responsible for transmitting discomfort to the brain.
In the lumbar spine, the nerves run in the spinal canal. When the nerve leaves the spinal canal it branches into a ventral root that goes to the leg (sciatic nerve) and a dorsal root that goes to the muscles of the back for motor function and the facets (joints of the spine) for sensation. It is these sensory fibers off the dorsal root that go to the facet that give you back pain in many situations. So, in patients that have mostly bad back pain and NOT a lot of leg pain, targeting those sensory fibers is a great way to reduce or eliminate back pain.
So if you have mostly back pain and minimal leg pain (sciatica) and the sensory nerves to the facets are the main source of that pain, RFA is a great choice for you.
Clinical Applications
One of the most common uses of radiofrequency ablation is in chronic pain management, particularly for conditions involving the spine. Patients with facet joint arthritis in the cervical, thoracic, or lumbar spine may benefit from RFA after diagnostic nerve blocks confirm the source of pain. RFA is also used to treat sacroiliac joint pain and certain types of knee pain.
In cardiology, radiofrequency ablation is widely used to treat abnormal heart rhythms (arrhythmias) such as atrial fibrillation. In this setting, catheters are guided into the heart to ablate small areas of tissue that trigger or sustain irregular electrical signals. My clinic does not offer this.
Procedure & Recovery
Radiofrequency ablation is typically performed under local anesthesia with imaging guidance such as fluoroscopy, ultrasound, or CT scanning. Patients are usually awake or lightly sedated in some settings, we do NOT sedate. The procedure often takes less than an hour, and most patients return home the same day.
You are prone on the procedure table and you are awake and not sedated. We numb up the skin where the needles and probes will go. We advance the probes to the location where the sensory nerves go to the facet and confirm that location both on fluoroscopy as well as with electrical testing. Then we anesthetize the area where the probe tip is with long acting numbing medication and give that about 5 minutes to take effect. Then we apply carefully controlled radio frequency energy via the probe to deliberately damage the sensory nerves to the facet so it cannot send pain signals. We apply that energy for about 90 seconds. Then we remove the probe.
Recovery is generally quick, with mild soreness or swelling at the treatment site lasting a few days. Pain relief may not be immediate; it can take several weeks for the full effect to be realized as the treated nerve fibers fully stop transmitting pain signals.
Benefits & Limitations
The primary advantages of radiofrequency ablation include its minimally invasive nature, reduced recovery time, and the potential for long-lasting relief—often six months to two years in pain management applications. However, RFA is not a permanent cure. Nerves can regenerate over time, and symptoms may recur, requiring repeat treatment. As with any procedure, risks such as infection, bleeding, or unintended nerve injury exist, though they are uncommon. It is often said that 90% of well selected patients get 60% better and 60% of patients get 90% better with RFA.
Remember, RFA is a great treatment for back pain that comes from facet branches off the dorsal spinal nerve. It is not very effective at all for leg pain or back pain that is NOT from the facets.
RFA is generally limited in use for postoperative patients if they have hardware, as the metal hardware can cause the radio frequency energy to concentrate or conduct into the wrong place.
Conclusion
Radiofrequency ablation is a versatile and effective medical technique that has transformed the treatment of chronic pain and other conditions across multiple specialties. By precisely targeting problematic nerves or tissues, RFA offers meaningful symptom relief with minimal disruption to patients’ lives, making it an important option in modern, minimally invasive medicine.